Attenuation of X-rays (AQA A Level Physics): Revision Note
Exam code: 7408
Attenuation of X-rays in Matter
When a collimated beam of X-rays passes through a patient’s body, the X-ray photons are absorbed and scattered
Different materials absorb X-rays by different amounts
For example, bones absorb a large proportion of X-ray photons which is why they appear bright white on an X-ray image
As the X-rays pass through a material, the intensity of the beam is found to decay exponentially
This decrease in intensity is known as attenuation
The attenuation of X-rays can be calculated using the equation:
Where:
= the intensity of the incident beam (W m-2)
= the intensity of the transmitted beam (W m-2)
= the linear absorption coefficient (m-1)
= distance travelled through the material (m)
The linear attenuation coefficient
is defined as
The fraction of X-rays removed per unit thickness of the material for a specified energy of the X-rays
The value of μ depends on the density of a substance and the energy of the X-ray photons
The greater the density of a material, the greater the value of μ
For example, bone absorbs a greater proportion of X-rays than soft tissue due to its higher density
Absorption of X-rays by flesh and bone
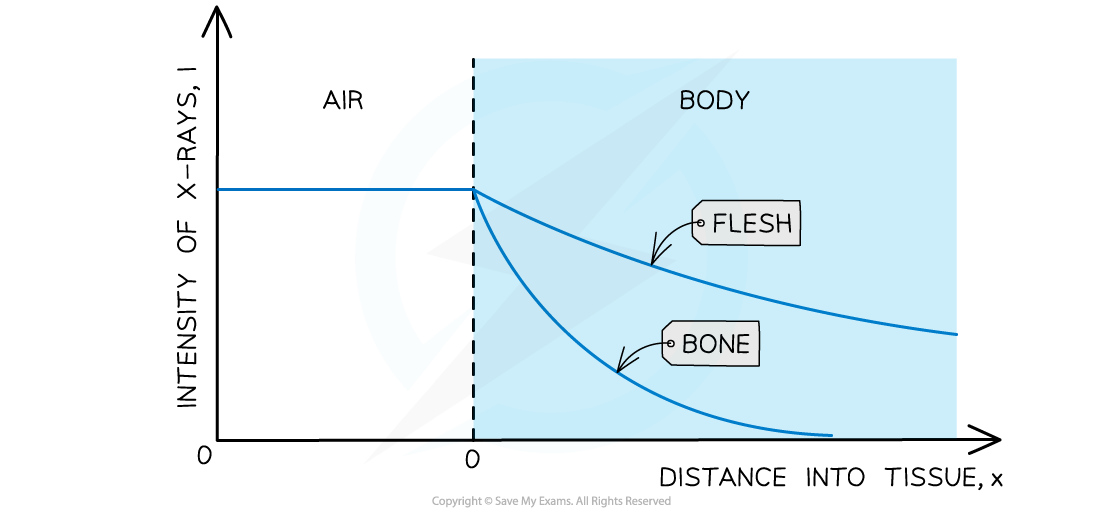
Bone is denser than soft tissues, such as flesh, so X-rays are absorbed more over a shorter distance
Half-value thickness
Similar to half-life in radioactivity, a material's ability to absorb X-rays is known as its half-value thickness
The half-value thickness of a material can be defined as:
The thickness of the material which will reduce the intensity of X-rays to half its original level for a specified energy of the X-rays
If the half-value thickness is
, then intensity has a value of
, so substituting this into the attenuation equation gives:
Taking natural logarithms of both sides gives
Hence, the half-value thickness of a substance is given by:
Worked Example
A student investigates the absorption of X-ray radiation in a model arm. A cross-section of the model arm is shown in the diagram.
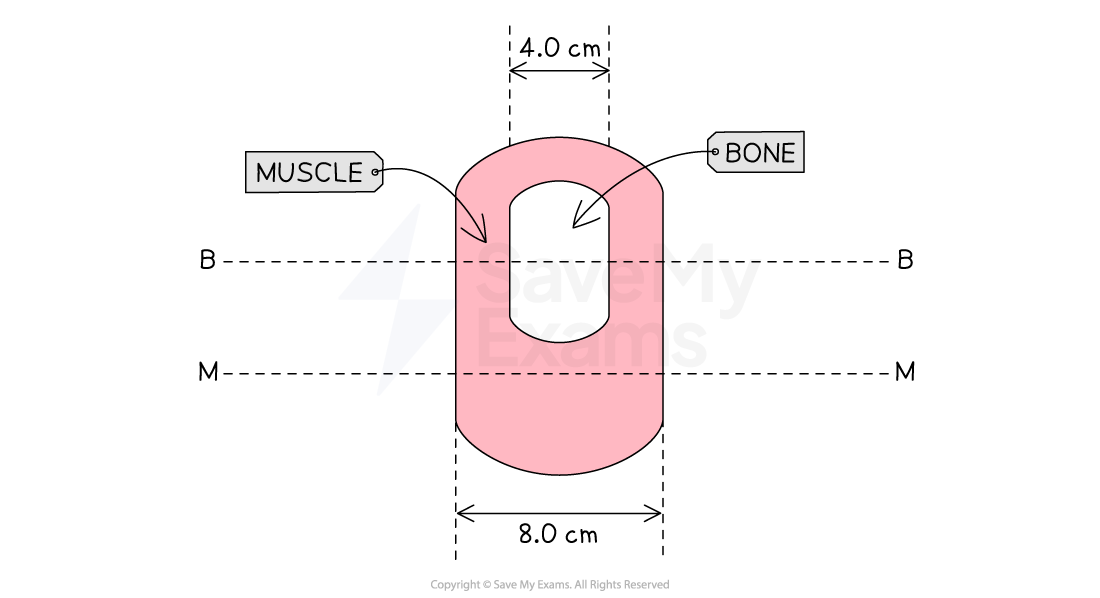
Parallel X-ray beams are directed along line MM and line BB. The linear absorption coefficients of the muscle and the bone are 0.20 cm−1 and 12 cm−1 respectively.
Calculate the ratio:
for a parallel X-ray beam directed along
(a) line MM
(b) line BB
and state whether the X-ray images have good contrast.
Answer:
Part (a)
Step 1: Write out the known quantities
Linear absorption coefficient for muscle,
= 0.20 cm-1
Distance travelled through the muscle,
= 8.0 cm
Step 2: Write out the equation for attenuation and rearrange
Where
= the intensity of the incident X-ray beam from the model
And
= the intensity of the incident X-ray beam on the model
Step 3: Substitute in values and calculate the ratio
Part (b)
Step 1: Write out the known quantities
Linear absorption coefficient for muscle,
= 0.20 cm-1
Linear absorption coefficient for bone,
= 12 cm-1
Distance travelled through the muscle,
= 4.0 cm
Distance travelled through the bone,
= 4.0 cm
Step 2: Write out the equation for attenuation for two media and rearrange
Step 3: Substitute in values and calculate the ratio
Step 4: Write a concluding statement
Each ratio gives a measure of the amount of transmission of the beam from the model
A good contrast is when:
There is a large difference between the intensities
The ratio is much less than 1.0
Therefore, both images have a good contrast
Differential Tissue Absorption
The amount of attenuation of a beam of X-rays depends on
the density of the absorbing tissue
the energy of the X-ray photons
The linear attenuation coefficient μ of an absorber is proportional to the density ρ of the absorbing substance
The higher the density of a material, the more X-ray energy that it absorbs
This is because the photons interact with more atoms, or a larger mass of atoms, in the same volume
Therefore, dividing the value of μ of a material by its density gives a constant value for that particular substance
This constant is known as the mass attenuation coefficient
Where:
= mass attenuation coefficient (m2 kg–1)
= linear attenuation coefficient (m–1)
= density of the absorbing material (kg m–3)
The mass attenuation coefficient of a substance describes how easily a beam of X-rays of a certain energy can penetrate it
The greater the mass attenuation coefficient, the stronger the absorption of X-rays by the material
The lower the mass attenuation coefficient, the greater the penetration of X-rays through the material
Mass attenuation coefficients for common elements
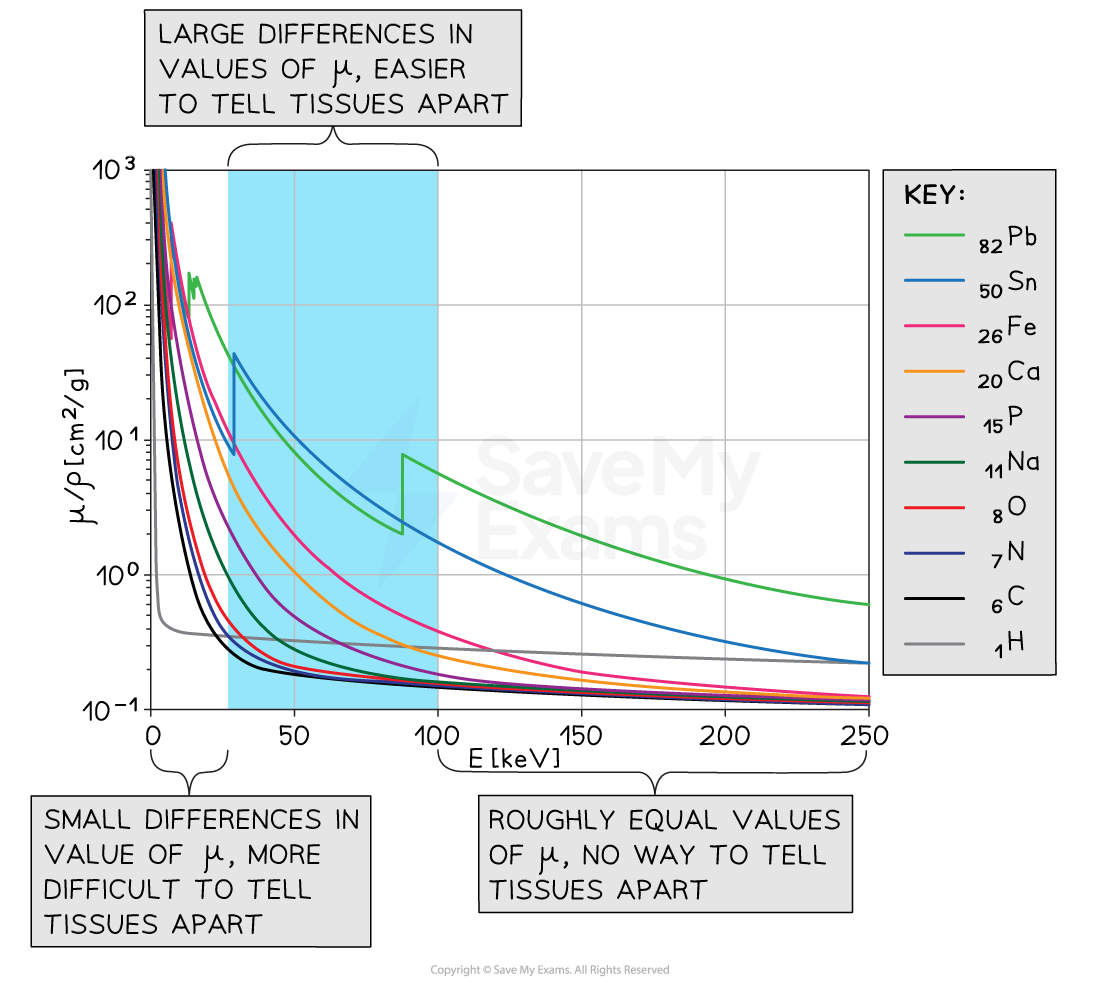
At very high and very low X-ray energies, differences in attenuation are very small. The optimum range for distinguishing different tissues is 30 keV to 100 keV
Photons of energies less than 30 keV...
are absorbed by soft tissue and bone
Therefore, these photons are removed from the X-ray beam by placing a suitable metal filter (e.g. lead or tin) in the path of the X-ray beam
Photons of energies between 30 keV and 100 keV...
are absorbed more readily by bone than by soft tissue
This is because the elements in bone have higher atomic numbers than the elements in soft tissues so bone can absorb photons in this energy range more readily
Therefore, these photons are used to distinguish between soft tissue and bone
Photons of energies greater than 100 keV...
are absorbed more equally in all types of tissue, including bone
This means they produce no distinction between any tissues
Therefore, these photons are not used in diagnostic X-ray imaging
Attenuation in different elements
The graph of mass attenuation coefficient and X-ray photon energy for elements with different values of atomic number Z shows that
Elements with lower Z values tend to absorb a lower proportion of X-rays
Elements with higher Z values tend to absorb a greater proportion of X-rays
The table below shows the composition of different substances and the effect of atomic number on attenuation
Substance | Elements | Effect on attenuation |
|---|---|---|
soft tissue | hydrogen | lower Z values, less attenuation |
bone | hydrogen | higher Z values, more attenuation |
contrast media | iodine | very high Z values, very large attenuation ideal for improving contrast |
heavy metals | lead | very high Z values, high attenuation at lower energies ideal for use as metal filters |
Worked Example
A monochromatic beam of X-rays passes through an aluminium sheet of thickness 2.5 mm. The intensity of the beam is reduced by 25%.
Calculate the mass attenuation coefficient for these X-rays.
The density of aluminium is 2700 kg m−3
Answer:
Step 1: List the known quantities:
Intensity of X-ray beam,
Thickness of aluminium sheet,
= 2.5 mm = 0.0025 m
Density of aluminium,
= 2700 kg m−3
Step 2: Determine the linear attenuation coefficient of the X-rays
Take natural logs of both sides:
linear attenuation coefficient: = 115 m−1
Step 3: Determine the mass attenuation coefficient of the X-rays
mass attenuation coefficient: = 0.043 m2 kg−1
Worked Example
The table shows the linear attenuation coefficients for bone and muscle at three different X-ray photon energies.
Photon energy / keV | Bone μ / cm–1 | Muscle μ / cm–1 |
30 | 2.13 | 0.41 |
50 | 0.68 | 0.24 |
80 | 0.36 | 0.20 |
100 | 0.30 | 0.18 |
Determine the energy of X-ray photons that would produce an image of muscle next to bone with the best contrast.
Answer:
Step 1: Recall the factor that determines the quality of contrast
Contrast depends on the difference in attenuation
The smaller the difference in attenuation, the poorer the contrast
The larger the difference in attenuation, the better the contrast
Step 2: Determine the difference between the values of attenuation at each energy
At 30 keV, the difference in attenuation is 2.13 − 0.41 = 1.72 cm–1
At 50 keV, the difference in attenuation is 0.68 − 0.24 = 0.44 cm–1
At 80 keV, the difference in attenuation is 0.36 − 0.20 = 0.16 cm–1
At 100 keV, the difference in attenuation is 0.30 − 0.18 = 0.12 cm–1
The difference between µ of bone and muscle is greatest using 30 keV X-rays hence this energy would produce an image with the best contrast

Unlock more, it's free!
Did this page help you?