Formation of Urine (Cambridge (CIE) A Level Biology): Revision Note
Exam code: 9700
Formation of urine in the nephron
The nephron is the functional unit of the kidney
The nephrons are responsible for the formation of urine
The process of urine formation in the kidneys occurs in two stages:
Ultrafiltration
Selective reabsorption
Stage | Name of process | Where process occurs | Explanation of process |
|---|---|---|---|
1 | Ultrafiltration | Bowman's capsule | Small molecules (including amino acids, water, glucose, urea and inorganic ions) are filtered out of the blood capillaries of the glomerulus and into the Bowman's capsule to form filtrate known as glomerular filtrate |
2 | Selective reabsorption | Proximal convoluted tubule | Useful molecules are taken back (reabsorbed) from the filtrate and returned to the blood as the filtrate flows along the nephron |
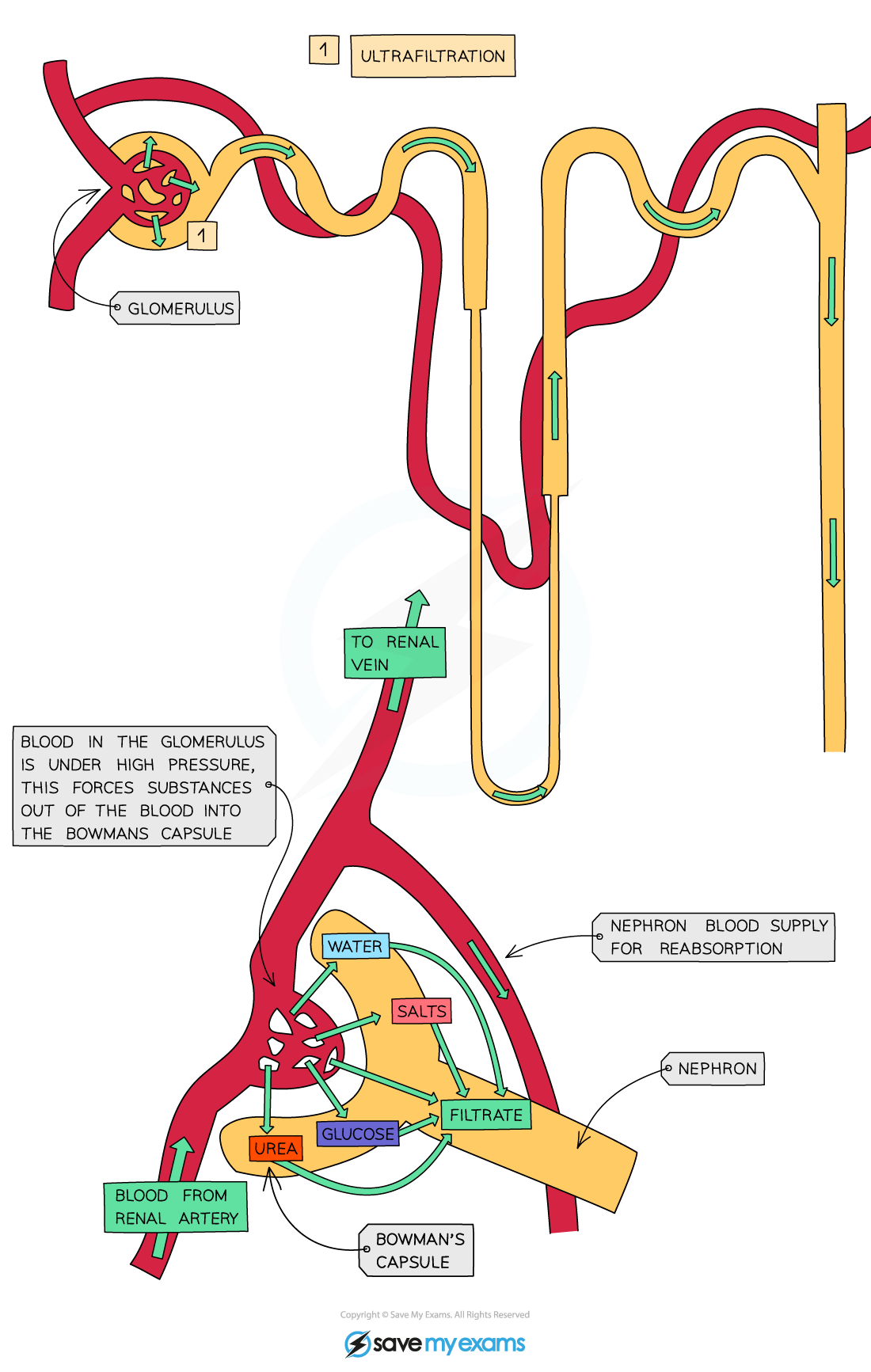
After the necessary reabsorption of amino acids, water, glucose and inorganic ions is complete, the filtrate eventually leaves the nephron and is now referred to as urine
This urine then flows out of the kidneys, along the ureters and into the bladder, where it is temporarily stored
Ultrafiltration
Arterioles branch off the renal artery and lead to each nephron, where they form a knot of capillaries (the glomerulus) sitting inside the cup-shaped Bowman’s capsule
The capillaries get narrower as they get further into the glomerulus which increases the pressure on the blood moving through them
This blood is already at high pressure because it is coming directly from the renal artery which is connected to the aorta)
This eventually causes the smaller molecules being carried in the blood to be forced out of the capillaries and into the Bowman’s capsule, where they form what is known as the filtrate
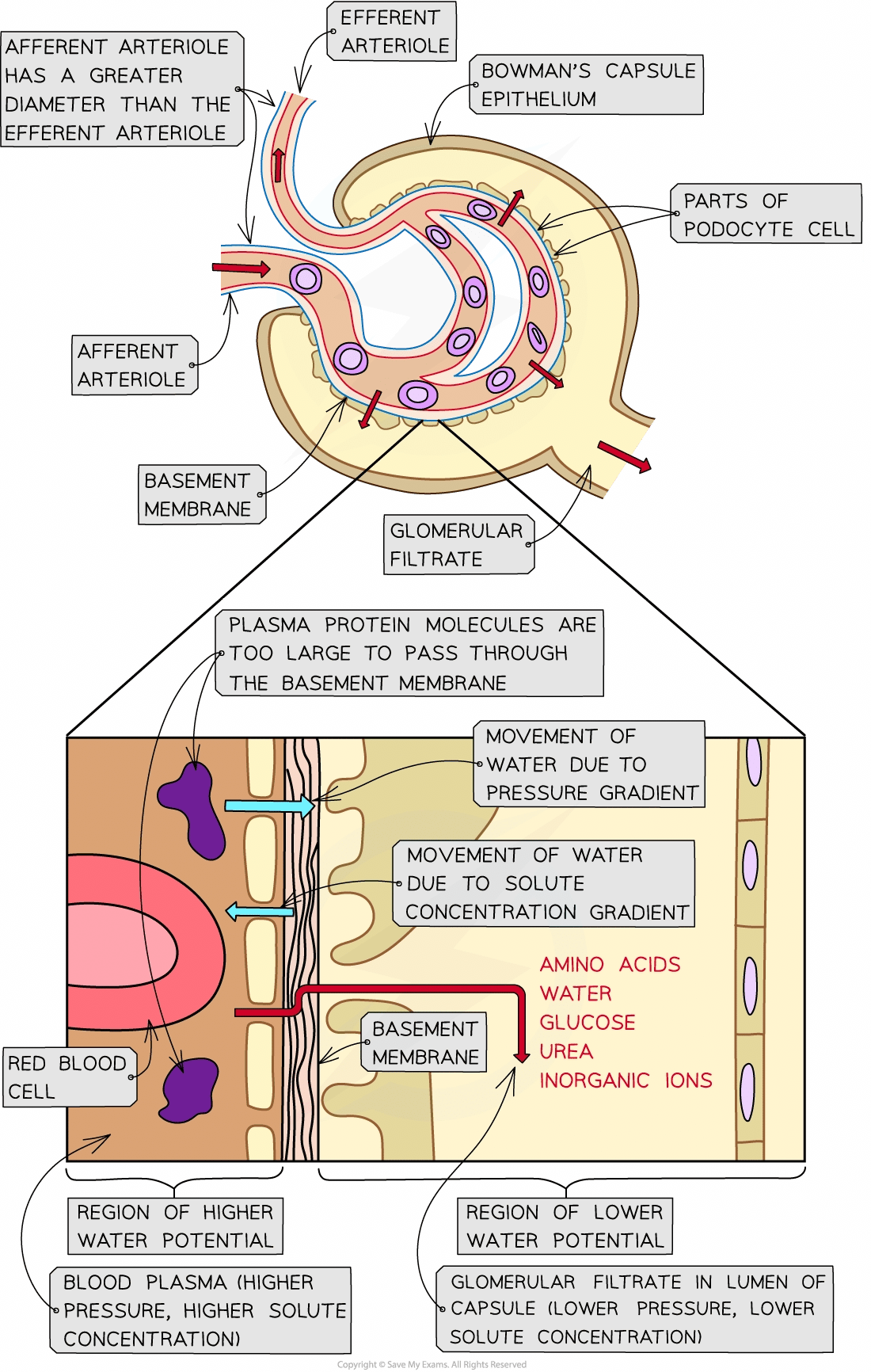
The blood in the glomerular capillaries is separated from the lumen of the Bowman’s capsule by two cell layers with a basement membrane in between them:
The first cell layer is the endothelium of the capillary—each capillary endothelial cell is perforated by thousands of tiny membrane-lined circular holes
The next layer is the basement membrane—this is made up of a network of collagen and glycoproteins
The second cell layer is the epithelium of the Bowman’s capsule—these epithelial cells have many tiny finger-like projections with gaps in between them and are known as podocytes
As blood passes through the glomerular capillaries, the holes in the capillary endothelial cells and the gaps between the podocytes allows substances dissolved in the blood plasma to pass into the Bowman’s capsule
The fluid that filters through from the blood into the Bowman’s capsule is known as the glomerular filtrate
The main substances that pass out of the capillaries and form the glomerular filtrate are: amino acids, water, glucose, urea and inorganic ions (mainly Na+, K+ and Cl-)
Red and white blood cells and platelets remain in the blood as they are too large to pass through the holes in the capillary endothelial cells
The basement membrane acts as a filter as it stops large protein molecules from getting through

How ultrafiltration occurs
Ultrafiltration occurs due to the differences in water potential between the plasma in the glomerular capillaries and the filtrate in the Bowman’s capsule
Water moves down a water potential gradient, from a region of higher water potential to a region of lower water potential
Water potential is increased by high pressure and decreased by the presence of solutes
Factor affecting water potential | How factor affects water potential in the glomerulus and Bowman’s capsule | Resulting movement of water |
|---|---|---|
Pressure | As the afferent arteriole is wider than the efferent arteriole, the blood pressure is relatively high in the glomerular capillaries This raises the water potential of the blood plasma in the glomerular capillaries above the water potential of the filtrate in the Bowman’s capsule | Water moves down the water potential gradient, from the blood plasma in the glomerular capillaries into the Bowman’s capsule |
Solute concentration | Whilst the basement membrane allows most solutes within the blood plasma to filter into the Bowman’s capsule, plasma protein molecules are too big to get through and stay in the blood As a result, the solute concentration in the blood plasma in the glomerular capillaries is higher than that in the filtrate in the Bowman’s capsule This makes the water potential of the blood plasma lower than that of the filtrate in the Bowman’s capsule | Water moves down the water potential gradient from the Bowman’s capsule into the blood plasma in the glomerular capillaries |
Overall, the effect of the pressure gradient outweighs the effect of solute gradient
Therefore, the water potential of the blood plasma in the glomerulus is higher than the water potential of the filtrate in the Bowman’s capsule
This means that as blood flows through the glomerulus, there is an overall movement of water down the water potential gradient from the blood into the Bowman’s capsule
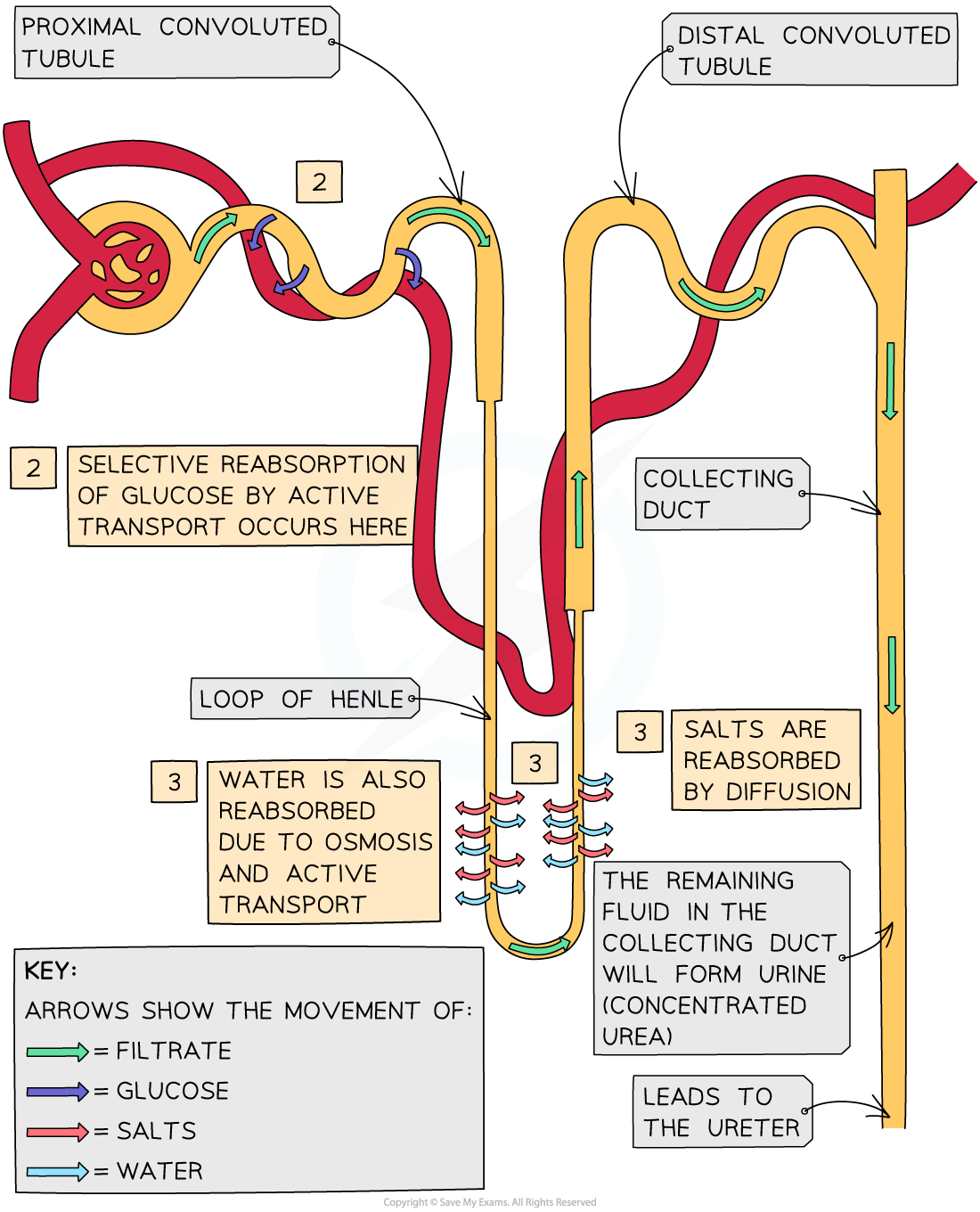
Selective reabsorption
Many of the substances that end up in the glomerular filtrate actually need to be kept by the body
These substances are reabsorbed into the blood as the filtrate passes along the nephron
This process is knowns as selective reabsorption as only certain substances are reabsorbed
Glucose reabsorption occurs in the proximal convoluted tubule
The lining of the proximal convoluted tubule is composed of a single layer of epithelial cells, which are adapted to carry out reabsorption in several ways:
Microvilli
Co-transporter proteins
A high number of mitochondria
Tightly packed cells
Water and salts are reabsorbed via the Loop of Henle and collecting duct
Adaptation of proximal convoluted tubule epithelial cell | How adaptation aids reabsorption |
|---|---|
Many microvilli present on the luminal membrane (the cell surface membrane that faces the lumen) | This increases the surface area for reabsorption |
Many co-transporter proteins in the luminal membrane | Each type of co-transporter protein transports a specific solute (e.g. glucose or a particular amino acid) across the luminal membrane |
Many mitochondria | These provide energy for sodium-potassium (Na+-K+) pump proteins in the basal membranes of the cells |
Cells tightly packed together | This means that no fluid can pass between the cells (all substances reabsorbed must pass through the cells) |
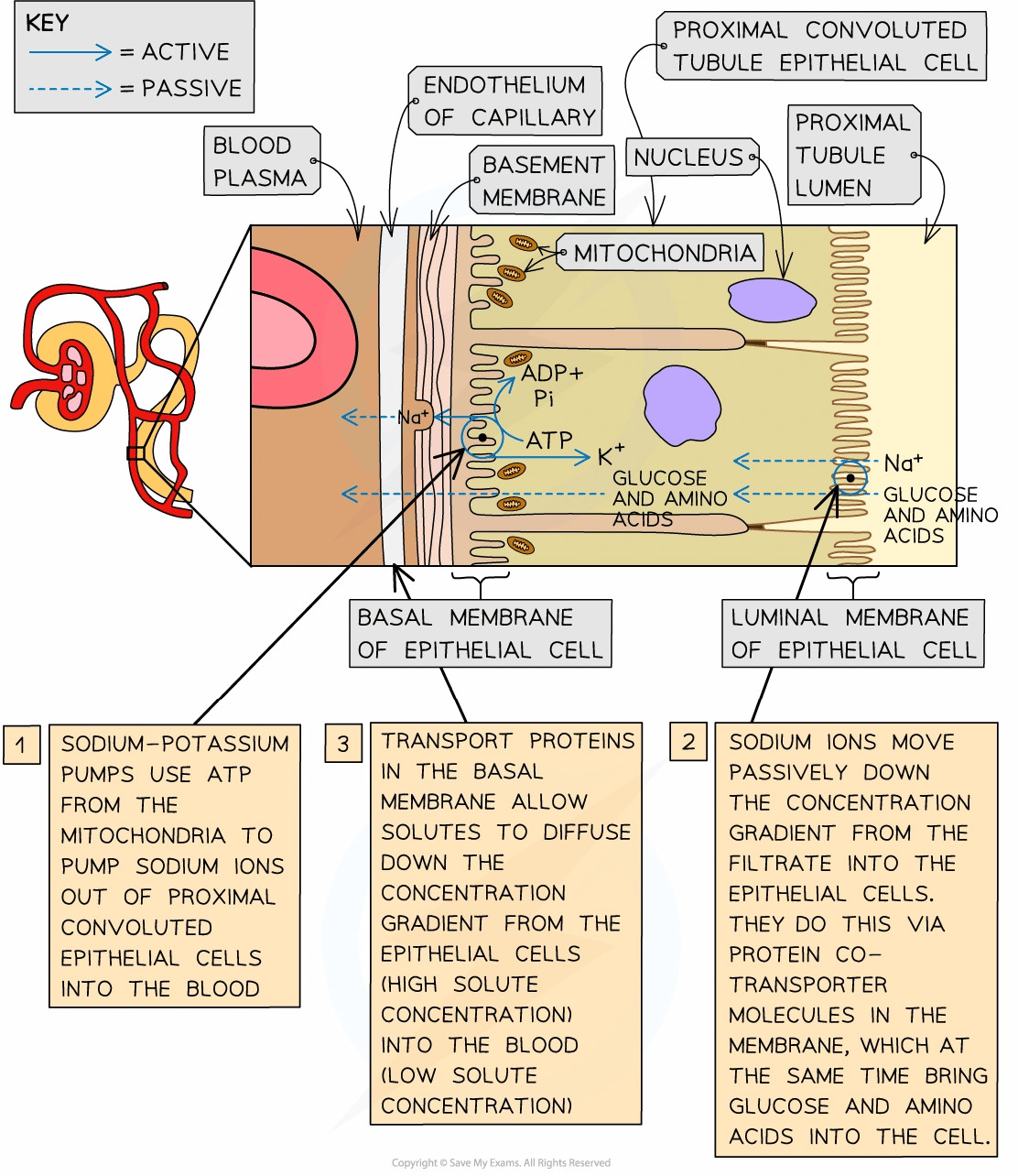
How the selective reabsorption of solutes occurs
Blood capillaries are located very close to the outer surface of the proximal convoluted tubule
As the blood in these capillaries comes straight from the glomerulus, it has very little plasma and has lost much of its water, inorganic ions and other small solutes
The basal membranes (of the proximal convoluted tubule epithelial cells) are the sections of the cell membrane that are closest to the blood capillaries
Sodium-potassium pumps in these basal membranes move sodium ions out of the epithelial cells and into the blood, where they are carried away
This lowers the concentration of sodium ions inside the epithelial cells
This causes sodium ions in the filtrate to diffuse down their concentration gradient through the luminal membranes (of the epithelial cells)
These sodium ions do not diffuse freely through the luminal membranes
They must pass through co-transporter proteins in the membrane
There are several types of these co-transporter proteins
Each type transports a sodium ion and another solute from the filtrate (e.g., glucose or a particular amino acid)
Once inside the epithelial cells, these solutes diffuse down their concentration gradients, passing through transport proteins in the basal membranes (of the epithelial cells) into the blood
Molecules reabsorbed from the proximal convoluted tubule during selective reabsorption
All glucose in the glomerular filtrate is reabsorbed into the blood
This means no glucose should be present in the urine
Amino acids, vitamins and inorganic ions are reabsorbed
The movement of all these solutes from the proximal convoluted tubule into the capillaries increases the water potential of the filtrate and decreases the water potential of the blood in the capillaries
This creates a steep water potential gradient and causes water to move into the blood by osmosis
A significant amount of urea is reabsorbed too
The concentration of urea in the filtrate is higher than in the capillaries, causing urea to diffuse from the filtrate back into the blood
Reabsorption of water and salts
As the filtrate drips through the Loop of Henle necessary salts are reabsorbed back into the blood by diffusion
As salts are reabsorbed back into the blood, water follows by osmosis
Water is also reabsorbed from the collecting duct in different amounts depending on how much water the body needs at that time

Unlock more, it's free!
Did this page help you?